- A DAP note is to be filled out each time you meet with a client for a CLEAR session. Please use the questions and statements listed below each section as a guide to what information needs to be included in order to ensure that this note is a complete explanation of the information shared during the session. Specific, FACTUAL information.
- Jun 23, 2014 For example, I will want a larger space to take notes on the interventions that I have done, as compared to documenting the goal of the session. After choosing a font, I modify the text so it is large and transparent (I tell InDesign to make it 40% transparent so I can write over these prompts).
- Data Assessment Plan (DAP) Note. CLIENT/ID: Date: Counselor’s Initials: A DAP note is to be filled out each time you meet with a client for a CLEAR session. Please use the questions and statements listed below each section as a guide to what information needs to be included in order to ensure that this note is a complete explanation of the.
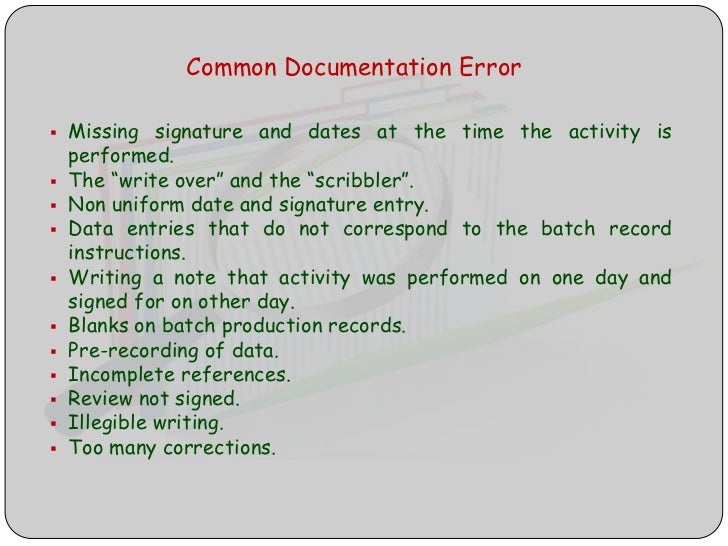
Does the note connect to the client’s individualized treatment plan? Are client strengths/limitations in achieving goals noted and considered? Is the note dated, signed and legible? Is the client name and/or identifier included on each page? Has referral and collateral information been documented?
This is the third post in a series that highlights standardized formats for your clinical notes. The series began here.
A second format for documenting your clinical work is called DA(R)P notes, sometimes referred to as DAP notes. These are similar to clinical SOAP notes.
DA(R)P is a mnemonic that stands for Data, Assessment (and Response), and Plan.
Data, in this format, includes both subective and objective data about the client as well as the therapist’s observations and all content and process notes from the session.
The Assessment and Response includes your clinical impressions, hunches, hypotheses, and rationale for your professional judgment. Progress is also noted here.
Plan refers to your original treatment plan and any response / revisions needed based on your most recent interactions with your client.
This method of clinical note taking is also an acceptable format for your documentation.
Darp Notes Examples
Tomorrow I’ll talk to you about BASIC SID notes.